Call Us
+91 8848318616
Get Appointment
Contact Now
Have More Questions
-
How often should I visit my dentist?
On average, seeing a dentist twice a year works well for many people. Some can get away with fewer visits. Others may need more frequent visits. People with very little risk of cavities or gum disease can do fine seeing their dentist just once a year. People with a high risk of dental disease might need to visit every three or four months, or more. This high-risk group includes:
- Smokers
- Pregnant women
- Diabetics
- People with current gum disease
- People with a weak immune response to bacterial infection
- People who tend to get cavities or build up plaque
The schedule for any person may change during a lifetime. In times of stress or illness, you may need to see the dentist more often than usual. The dentist may help you to fight off a temporary infection or treat changes in your mouth.
If you take good care of your teeth and gums at home and your dentist doesn't find any cavities or gum disease for a few years, he or she may choose to lengthen the time between visits. Ask your dentist the best schedule for your routine dental visits.
-
Is age a criteria for orthodontic treatment?
Ideally, human teeth would line up as neatly as the keys on a piano. Unfortunately, many people must contend with crooked teeth, crowded smiles, or poorly aligned bites.
These problems raise more than cosmetic concerns. Crowded or overlapping teeth can be difficult to clean, making tooth decay and gum disease more likely. Teeth that don't come together properly when you close your jaws—a problem called malocclusion, or "bad bite"—can cause chewing and swallowing problems. Poor tooth alignment can also make it difficult to pronounce certain sounds and can put excessive stress on the chewing muscles, causing facial pain.
Although childhood is the ideal time to make changes in the positioning of the teeth, more adults are opting for orthodontic treatment and coming away with excellent results.
Simply put, there is actually no age limit for someone to get braces. According to the American Association of Orthodontists, there is a high number of patients fitted with dental braces every day over the age of 18. Typically, the only requirements dental professionals have is a healthy jaw bone and permanent teeth.
-
Is It Safe To Go To the Dentist During Pregnancy?
In between trips to the doctor, hospital tours and setting up the nursery, don’t let visiting the dentist fall off your pregnancy to-do list before your baby comes. Getting a checkup during pregnancy is safe and important for your dental health. Not only can you take care of cleanings and procedures like cavity fillings before your baby is born, but your dentist can help you with any pregnancy-related dental symptoms you might be experiencing.
Here are some common concerns women have about going to the dentist during pregnancy.
When to Tell Your Dentist You Are Pregnant
Even if you only think you might be pregnant, let your dental office know. Tell them how far along you are when you make your appointment. Also let your dentist know about the medications you are taking or if you have received any special advice from your physician. If your pregnancy is high-risk or if you have certain medical conditions, your dentist and your physician may recommend that some treatments be postponed.
How Pregnancy Will Affect Your Mouth?
Although many women make it nine months with no dental discomfort, pregnancy can make some conditions worse – or create new ones. Regular checkups and good dental health habits can help keep you and your baby healthy.
Pregnancy Gingivitis
Your mouth can be affected by the hormonal changes you will experience during pregnancy. For example, some women develop a condition known as “pregnancy gingivitis,” an inflammation of the gums that can cause swelling and tenderness. Your gums also may bleed a little when you brush or floss. Left untreated, gingivitis can lead to more serious forms of gum disease. Your dentist may recommend more frequent cleanings to prevent this.
Increased Risk of Tooth Decay
Pregnant women may be more prone to cavities for a number of reasons. If you’re eating more carbohydrates than usual, this can cause decay. Morning sickness can increase the amount of acid your mouth is exposed to, which can eat away at the outer covering of your tooth (enamel).
Brushing twice a day and flossing once can also fall by the wayside during pregnancy for many reasons, including morning sickness, a more sensitive gag reflex, tender gums and exhaustion. It’s especially important to keep up your routine, as poor habits during pregnancy have been associated with premature delivery, intrauterine growth restriction, gestational diabetes and preeclampsia.
Pregnancy Tumors
In some women, overgrowths of tissue called “pregnancy tumors” appear on the gums, most often during the second trimester. It is not cancer but rather just swelling that happens most often between teeth. They may be related to excess plaque. They bleed easily and have a red, raw-looking raspberry-like appearance. They usually disappear after your baby is born, but if you are concerned, talk to your dentist about removing them.
Medications
Be sure your dentist knows what, if any, prescription medications and over-the-counter drugs you are taking. This information will help your dentist determine what type of prescription, if any, to write for you. Your dentist can consult with your physician to choose medications—such as pain relievers or antibiotics—you may safely take during the pregnancy. Both your dentist and physician are concerned about you and your baby, so ask them any questions you have about medications they recommend.
Local Anesthetics During Pregnancy
If you’re pregnant and need a filling, root canal or tooth pulled, one thing you don’t have to worry about is the safety of the numbing medications your dentist may use during the procedure. They are, in fact, safe for both you and your baby.
A study in the August 2015 issue of the Journal of the American Dental Association followed a group of pregnant women who had procedures that used anesthetics like lidocaine shots and a group that did not. The study showed these treatments were safe during pregnancy, as they cause no difference in the rate of miscarriages, birth defects, prematurity or weight of the baby. “Our study identified no evidence to show that dental treatment with anesthetics is harmful during pregnancy,” said study author Dr. Hagai. “We aimed to determine if there was a significant risk associated with dental treatment with anesthesia and pregnancy outcomes. We did not find any such risk.”
Dental X-Rays During Pregnancy
Yes, it's safe to get an X-ray during pregnancy. Although radiation from dental X-rays is extremely low, your dentist or hygienist will cover you with a leaded apron that minimizes exposure to the abdomen. Your dental office will also cover your throat with a leaded collar to protect your thyroid from radiation.
-
My child is having thumbsucking even at the age of 6,is there any treatment for that?
Thumb sucking is a common habit among children. At some point, though, you might think, "Enough is enough." Here's help encouraging your child to stop the behavior.
Why do some children suck their thumbs?
Babies have natural rooting and sucking reflexes, which can cause them to put their thumbs or fingers into their mouths — sometimes even before birth. Because thumb sucking makes babies feel secure, some babies might eventually develop a habit of thumb sucking when they're in need of soothing or going to sleep.
How long does thumb sucking usually last?
Many children stop sucking their thumbs on their own, often by age 6 or 7 months or between ages 2 and 4.
But even a child who's stopped sucking his or her thumb might go back to the behavior during times of stress.
When should I intervene?
Thumb sucking isn't usually a concern until a child's permanent teeth come in. At this point, thumb sucking might begin to affect the roof of the mouth (palate) or how the teeth line up. The risk of dental problems is related to how often, how long and how intensely your child sucks on his or her thumb.
Although some experts recommend addressing sucking habits before age 3, the American Academy of Pediatrics says treatment is usually limited to children who continue thumb sucking after turning 5.
What can I do to encourage my child to stop thumb sucking?
Talk to your child about thumb sucking. You're more likely to be successful in stopping the habit if your child wants to stop and helps choose the method involved.
Sometimes paying no attention to thumb sucking is enough to stop the behavior — especially if your child uses thumb sucking to get attention. If ignoring it isn't effective, try one of these techniques:
- Use positive reinforcement. Praise your child or provide small rewards — such as an extra bedtime story or a trip to the park — when he or she isn't thumb sucking. Set attainable goals, such as no thumb sucking an hour before bed. Place stickers on a calendar to record the days when your child successfully avoids thumb sucking.
- Identify triggers. If your child sucks his or her thumb in response to stress, identify the real issue and provide comfort in other ways — such as with a hug or reassuring words. You might also give your child a pillow or stuffed animal to squeeze.
- Offer gentle reminders. If your child sucks his or her thumb without thought — rather than as a way to get attention — gently remind him or her to stop. Don't scold, criticize or ridicule your child.
Can the dentist help?
If you're concerned about the effect of thumb sucking on your child's teeth, check with the dentist. For some kids, a chat with the dentist about why it's important to stop thumb sucking is more effective than a talk with mom or dad.
Rarely, some doctors recommend using unpleasant techniques, such as covering your child's thumbnail with a bitter substance, bandaging the thumb or covering the hand with a sock at night.
What if nothing works?
For some children, thumb sucking is an incredibly difficult habit to break. Try not to worry. Putting too much pressure on your child to stop thumb sucking might only delay the process.
-
What is the cost for orthognathic surgery?
Orthognathic surgery is a corrective jaw surgery that straightens or realigns your jaw, and corrects related skeletal deformities that a patient may need. At minimum, orthognathic surgery cost includes surgeon fees, hospital fees, orthodontics charges, anesthesia fees and pain medications. However, final expenses may depend on a number of conditions unique to the person.
Jaw surgery, also known as orthognathic (or-thog-NATH-ik) surgery, corrects irregularities of the jaw bones and realigns the jaws and teeth to improve the way they work. Making these corrections may also improve your facial appearance.
Jaw surgery may be a corrective option if you have jaw problems that can't be resolved with orthodontics alone. In most cases, you also have braces on your teeth before surgery and during recovery after surgery until healing and alignment are complete. Your orthodontist can work with your oral and jaw and face (maxillofacial) surgeon to determine your treatment plan.
Jaw surgery is appropriate after growth stops, usually around ages 14 to 16 years for females and ages 17 to 21 years for males.
Why it's done
Jaw surgery may help to:
- Make biting and chewing easier and improve chewing overall
- Correct problems with swallowing or speech
- Minimize excessive wear and breakdown of the teeth
- Correct bite fit or jaw closure issues, such as when the molars touch but the front teeth don't touch (open bite)
- Correct facial imbalance (asymmetry), such as small chins, underbites, overbites and crossbites
- Improve the ability of the lips to fully close comfortably
- Relieve pain caused by temporomandibular joint (TMJ) disorder and other jaw problems
- Repair facial injury or birth defects
- Provide relief for obstructive sleep apnea
Risks
Jaw surgery is generally safe when done by an experienced oral and maxillofacial surgeon, often in collaboration with an orthodontist.
Risks of surgery may include:
- Blood loss
- Infection
- Nerve injury
- Jaw fracture
- Relapse of the jaw to the original position
- Problems with bite fit and jaw joint pain
- Need for further surgery
- Need for root canal therapy on selected teeth
- Loss of a portion of the jaw
After surgery, you may experience:
- Pain and swelling
- Problems with eating that can be addressed with nutritional supplements or consultation with a dietitian
- A brief time of adjustment to a new facial appearance
How you prepare
In most cases, an orthodontist places braces on your teeth before surgery. Braces are usually on for 12 to18 months before surgery to level and align your teeth in preparation for surgery.
Your orthodontist and oral and maxillofacial surgeon work together to develop your treatment plan. X-rays, pictures and models of your teeth are part of the planning for your jaw surgery. Occasionally, the difference in the way teeth fit together will require either reshaping of the teeth, covering the teeth with crowns or both to complete correction.
Three-dimensional CT scanning, computer-guided treatment planning and temporary orthodontic anchoring devices may be used to help in the movement of teeth and decrease your time in braces. Sometimes these efforts completely eliminate the need for jaw surgery.
Sometimes virtual surgical planning (VSP) will be used to guide your surgeon to fit and correct the jaw segment position during the procedure for the most optimal result.
What you can expect
Before the procedure
Jaw surgery is performed by oral and maxillofacial surgeons. Surgery is usually done under general anesthesia. Surgery takes place in the hospital and requires a two- to four-day stay.
During the procedure
Surgery usually can be performed inside your mouth, so no facial scars show on your chin, jaw or around the mouth. However, sometimes small incisions may be required outside your mouth.
Your surgeon makes cuts in the jawbones and moves them into the correct position. Once your jaw movement is completed, tiny bone plates, screws, wires and rubber bands may be used to secure the bones into their new position. These screws — which are smaller than a bracket used for braces — become integrated into the bone structure over time.
In some cases, extra bone may be added to the jaw. Your surgeon transfers the bone from your hip, leg or rib and secures it with plates and screws. In other cases, bone may be reshaped to provide a better fit.
Jaw surgery may be performed on the upper jaw, lower jaw, chin or any combination of these.
Upper jaw (maxillary osteotomy)

Upper jaw surgery
Surgery on the upper jaw may be performed to correct:
- Significantly receded or protruding upper jaw
- Crossbite
- Too much or too little of the teeth showing
- Open bite
- Reduced facial growth of the middle of the face (midfacial hypoplasia)
Your surgeon cuts the bone above your teeth so that the entire top jaw — including the roof of your mouth and your upper teeth — can move as one unit. The jaw and upper teeth are moved forward until they fit properly with the lower teeth. This can be planned on a computer to determine if additional work, such as orthodontics, will be needed to help correct any remaining fit difference.
An open bite occurs when excess bone grows above the molars, causing what's normally a flat, even surface to become angled. To fix this, your surgeon shaves away or removes the excess bone.
Once the jaw is realigned, plates and screws hold the bone in its new position.
Lower jaw (mandibular osteotomy)

Lower jaw surgery
A mandibular osteotomy can correct:
- Receding lower jaw
- Protruding lower jaw
The surgeon makes cuts behind the molars and lengthwise down the jawbone so the front of the jaw can move as one unit. The jaw can then be moved to its new position either forward or backward. Plates and screws hold the jawbone together as it heals.
Chin surgery (genioplasty)

Chin surgery
A genioplasty can correct a small chin (deficient chin). A small chin often accompanies a severely receded lower jaw.
Typically, surgeons can alter the jaw and restructure the chin during the same surgery. The surgeon cuts a piece of the chin bone on the front of the jaw, moves it forward, and secures it in a new position with plates and screws.
After the procedure
After surgery, your doctor will provide you with instructions. These usually include:
- What you can eat
- Oral hygiene
- Avoiding tobacco
- Avoiding strenuous activity
- Medications to control pain
- When to return to work or school, which is usually in one to three weeks
Initial jaw healing typically takes about six weeks after surgery, but complete healing can take up to 12 weeks.
After initial jaw healing — at about six weeks — your orthodontist finishes aligning your teeth with braces. The entire orthodontic process, including surgery and braces, may take several years. Once the braces are removed, retainers to hold tooth position may be used.
Results
Correcting alignment of your jaws and teeth with jaw surgery can result in:
- Balanced appearance of your lower face
- Improved function of your teeth
- Health benefits from improved sleep, breathing, chewing and swallowing
- Improvement in speech impairments
Secondary benefits of jaw surgery may include:
- Improved appearance
- Improved self-esteem
-
Wisdom teeth infection:what to do?
Can the dentist help?
Your wisdom teeth are molars. They’re the large teeth at the back of your mouth, sometimes called the third molars. They’re the last teeth to grow in. Most people get wisdom teeth between the ages of 17 and 25.
Like other teeth, a wisdom tooth can:
- decay
- get a cavity
- become impacted
- get stuck below or in the gumline
If you have a wisdom tooth infection, you’ll need treatment from a dentist. But not all pain is the result of a tooth infection. Below we discuss treatments for wisdom teeth infection and pain.
How infection occurs
Wisdom teeth may get infected because they’re harder to clean. Food and bacteria can get trapped between the tooth and the gums. The space between your wisdom teeth and the back of your mouth can be easy to miss when you’re brushing and flossing.
An impacted wisdom tooth may not grow through your gums correctly. It may partially emerge, grow in at an angle, or develop completely sideways.
A partially impacted wisdom tooth has a higher risk of infection. This is because its shape and angle make decay more likely to happen. A tooth infection or cavity happens when an overgrowth of bacteria makes holes in the outer, hard enamel layer.
Several kinds of bacteria can cause an infection in and around a wisdom tooth. In rare cases, the infection can spread to other areas of the mouth and head. Types of bacteria that can lead to a tooth infection include:
- Streptococcus
- Actinomyces
- Peptostreptococcus
- Prevotella
- Fusobacterium
- Aggregatibacter
- Eikenella corrodens
Treatments
Treatment for a wisdom tooth infection may involve:
- medication to treat the tooth
- dental work to repair it
- surgery for tooth removal
Your dentist will examine your teeth and take an X-ray of the area. This will help determine what kind of treatment is best for your tooth.
Removal
If your wisdom tooth is damaged, your dentist may completely or partly remove it. You may need dental surgery for an impacted wisdom tooth infection. Other impacted wisdom teeth may also be removed. This helps to prevent future infections.
Your dentist may remove gum tissue from the top of an impacted wisdom tooth to help it grow through. Another dental procedure removes only the top part of a wisdom tooth. This is called a coronectomy. This helps to protect the tooth roots, nerves, and the jawbone around the tooth.
Surgery facts
Pulling a wisdom tooth can be complicated. You’ll need local anesthesia by an injection in the area, or general anesthesia. The procedure may take 20 minutes or longer. Your dentist may need to section the tooth and remove it in pieces. This helps to avoid injury to the nerves and jawbone.
Possible side effects and risks after wisdom tooth removal surgery include:
- bleeding
- infection
- numbness in your tongue, lower lip, or chin
- jawbone weakness
An infection in the mouth can happen two weeks or even up to two months after getting a wisdom tooth removed. Let your dentist know about any symptoms. You may need another dose of antibiotics to treat it.
Home remedies
Home remedies can’t treat a wisdom tooth infection. However, some simple treatments may give you temporary relief from the pain and discomfort. Try these remedies if you have to wait to see your dentist.
- Salt water rinse. Mix salt in warm or cold drinking water. Swish it around your mouth a few times and spit out. The salt helps to temporarily slow down some of the bacteria.
When to see a doctor
Call your dentist and make an appointment if you have any pain or discomfort in or around a wisdom tooth. This area can be difficult to see. You’ll likely need a dental exam and an X-ray scan to find out what’s causing the pain.
Don’t ignore any teeth, gum, or jaw symptoms such as:
- pain or sensitivity
- tender or swollen gums
- red or bleeding gums
- white fluid or oozing around teeth
- bad breath
- bad taste in your mouth
- jaw pain
- jaw swelling
- stiff jaw
- difficulty breathing, opening your mouth, or speaking
You may also have a fever, chills, nausea, or headache pain because of a wisdom tooth infection.
The bottom line
You can’t prevent an impacted wisdom tooth. See your dentist for regular checkups to help prevent wisdom tooth complications.
Good dental hygiene, such as brushing and flossing several times a day, can help keep your wisdom teeth from getting infected.
-
What is the difference between bridge and implants??
What are Dental Implants?
This is a good option if you have lost a tooth or teeth to an injury, periodontal disease, or other reasons. A dental implant is a titanium post (acting as a tooth root) that supports a crown. It is surgically inserted into the jawbone where it will then fuse (or osseointegrate) into the jawbone to ensure that it is anchored in position. After the osseointegration process is finished (usually 3-6 months), an abutment is attached to the post frame. It protrudes above the gum line to provide the area where the dental crown is cemented or screwed into.
Types of Implants
Endosteal implants
Endosteal implants are directly implanted into the jawbone during surgery. A second surgery is needed to connect the post to the first implant once the gum tissue is healed. Last, an artificial tooth is mounted to the post.
Subperiosteal implants
With subperiosteal implants, a metal frame is fitted onto the jawbone right below the gum tissue. The frame becomes fixed to the jawbone as the gums heal. Once ready, the artificial tooth is attached to the post.
Pros and Cons of Dental Implants
Pros
- Little maintenance : One big perk about dental implants is that they can last a lifetime when they are high quality. They require little maintenance.
- Natural looking : Dental implants look, feel, and function like a natural tooth. They are strong and stable, and they keep your smile confident.
- Protect Your Jawbone : Having an open space in your mouth where a missing tooth once was puts your jawbone at risk for deterioration. Dental implants stimulate and preserve natural bone growth, which helps prevent bone loss.
- No Strain on Teeth : Unlike a bridge, an implant stands on it’s own support without putting strain on other teeth. This helps to protect surrounding teeth.
Cons
- Surgery : Because the implant must be attached to your bone, it requires surgery. And there are always risks to consider with any kind of surgical procedure. Some of the risks include infection, nerve damage, damage to surrounding teeth, jaw fractures, and more.
- Time : Getting a tooth implant is not something that can be done in a single office visit. Bone heals slowly, to the entire procedure can take several months, around 3 months on the fast end.
- Cost : Now, the cost will vary depending on the type of implant and the conditions of the tooth issue. Still, the high cost associated with getting a dental implant is often what deters people from considering this procedure.
What are Dental Bridges?
Dental bridges are used to bridge the gap between one or more missing teeth. The bridge is supported by the natural teeth or implants on either side. It is made up of two or more crowns for the teeth on each part of the gap. The anchoring teeth are called abutment teeth, and the false teeth that lie in between are called pontics.
Types of Bridges?
Traditional bridges
This type of bridge is most common one, and it’s usually made of either ceramics or porcelain fused to metal. The bridge is created by a crown for the tooth or implant on either side of the gap, and the pontic lies in between.
Cantilever Bridges
This type of bridge is not as common as the traditional bridge, and it is not recommended for the back of the mouth where it will receive much force. Cantilever bridges are used when there are adjacent teeth found on only one side of the gap of missing teeth.
Maryland Bonded Bridges
With this type of bridge, the resin-bonded bridge is made of porcelain, porcelain fused to metal, or plastic teeth supported by a porcelain or metal framework. The existing teeth on either side of the gap are bonded to the metal or porcelain wings on the bridge.
Pros and Cons of Dental Bridges
Pros
- Simple procedure : Unlike dental implants, bridges don’t require surgery, making bridges a lot less painful. All it takes is a simple dental procedure to get your teeth fixed.
- Faster : It’s much quicker and easier to get dental bridges (only a few weeks at the most), whereas implants may take several months.
- Affordable : Bridges are generally more affordable than implants, and they are still strong and supportive for your mouth.
Cons
- Less Aesthetically Pleasing : Bridges are not as natural looking as implants, and therefore are not as aesthetically pleasing.
- Periodic Replacement : Bridges need to be replaced periodically. They should be changed every 5-7 years.
- Damage Natural Teeth : Adjacent teeth undergo a lot of preparation that requires the removal of a considerable amount of tooth structure.
What should you choose?
Comparing the Costs
As you can see in the chart below, the price of a dental bridge can vary dramatically. Still, it may or may not end up being a more affordable option than a dental implant.
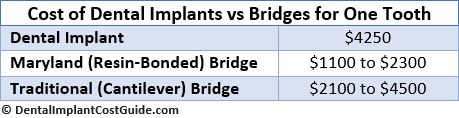
Other things to consider
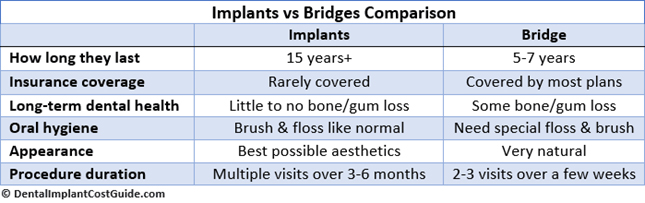
Dental Coverage
Are you covered for either one of these dental procedures? While bridges are usually covered by most dental insurance plans, implants are rarely covered. If you don’t have insurance or you want to find a more affordable option, you can consider joining a discount dental plan membership that provides discounted rates on these types of procedures.
Procedure Duration
How long are you willing to wait to have your teeth fixed? A bridge can be fixed in 2 or 3 visits to the dentist, having it done in no time. An implant is a long procedure that requires surgeries and recovery times over the span of several months.
Lifespan
The long lifespan and little maintenance associated with dental implants makes patients over the age of 40 good candidates for this procedure. They may need to be replaced every 15 years or so do to natural wear and tear. Bridges, while more affordable, must be replaced every 5-7 years, and possibly 10 years with the proper care and maintenance.
What works best for you will really depend on your unique situation. Everything from your access to affordable dental care, to the state of your oral health, to basic finances will ultimately determine whether you need a dental bridge or a dental implant.
-
Are Dental Crowns Needed After the Root Canal Procedure?
Root canal procedures primarily address the problem with a tooth which is infected or has a decaying pulp that requires urgent drilling and cleaning from inside. The integrity of your tooth is either lost or severely damaged after an invasive therapy like a root canal and you will need teeth reinforcement.
A dental crown after a root canal provides reinforcement to your tooth and restores its health and functionality. Although adding a dental crown is not necessary after every root canal procedure, all root canal procedures need tooth reinforcement.
Is a Dental Crown Necessary After a Root Canal?
Studies reveal that a dental crown following a root canal improves the chance of tooth survival. One study recorded a six times higher survival rate for teeth with dental crowns. Another study states that only about one-third of the molars endure without a crown for five years.
Here are some crucial reasons why adding dental crowns after root canal procedures are needed.
- Restore a Fragile Tooth : A tooth can turn more fragile after the root canal treatment due to tooth-drilling, cavity or infection. A durable dental crown can protect this tooth and make it long-lasting while preventing any damage.
- Protect a Tooth from Sensitivity : Following root canal therapy, some of the existing nerves may develop extra sensitivity to heat and cold which can be very uncomfortable. This is another reason why a dental crown is needed to protect a tooth after the root canal procedure.
- Retain a Natural-Looking Color : Some teeth change color after a root canal treatment. If a tooth appears grayed or deeply stained, a dental crown can offer a more natural appearance and whiter shade to match the remaining teeth.
- Prevent Infections : The affected tooth surface is at a higher risk of infection and contamination post a root canal therapy. A dental crown will protect the tooth by sealing it off from dangerous leakage to avoid recontamination so that you do not need to undergo a tooth extraction.
- Provide a Back-Up Security : A tooth that previously had a filling due to extensive decay and got chipped or fractured before the root canal treatment, or if it’s in a high traffic area should necessarily be restored with a dental crown.
- People who tend to get cavities or build up plaque
Which Teeth Require Dental Crown Following a Root Canal?
A simple way to find out if you require a tooth crown after root canal is to locate where the affected tooth is in your mouth. You typically need a dental crown after a root canal on your back grinding teeth, molars and premolars. Front teeth, canines, and incisors may not require a dental crown. Your dentist will decide whether a dental crown after a root canal is needed.
-
How often should I change my tooth brush???
Replace toothbrushes every 3 to 4 months. Consider getting a new toothbrushsooner if you have been sick, especially if the toothbrush is stored close to othertoothbrushes. When in doubt, look at the bristles.
-
I have bleeding from my gums when brushing what can be the reason?
Bleeding gums are caused by inadequate plaque removal. Plaque contains germs which attack the healthy tissue around the teeth. If plaque build-up occurs, gums become inflamed and irritated, which may cause them to bleed when brushing or flossing. This is called gingivitis and is the first stage of gum disease.
-
Can Scaling Damage Your Teeth Enamel? Know the Myths and Facts?
Scaling is a dental procedure recommended by dentists to be done regularly particularly twice a year. However, some people have their doubts about subjecting their teeth to this treatment, despite the many evidences proving otherwise. Read on as we take a look at the myths related to scaling and the real truth behind these misconceptions.
Myth: Scaling loosens teeth
Fact: Scaling can help strengthen the teeth’s hold on surrounding bone and gums.
Ultrasonic scaling, where its tip barely touches the teeth for a few seconds at a time cannot possibly loosen tooth. Your teeth will feel loose after scaling because tartar is tightly stuck around the teeth, that when they are removed, your teeth will naturally feel loose. A few weeks later once your gums heal, you will notice that your teeth actually feels firmer.
Myth: Scaling makes teeth sensitive
Fact: Scaling can prevent tooth sensitivity by preventing gum inflammation and recession
Think of tartar as a jacket worn over your teeth. It has been there for weeks and even months that suddenly removing it through scaling will require some time for your teeth to adjust to the new temperature. They have become sensitive; they only need time to recover. Of course, scaling done by untrained hands can lead to prolonged sensitivity; this is why you should choose a good dentist.
Myth: Scaling is a cosmetic procedure
Fact: Scaling is important for gum health; it is both cosmetic and therapeutic
The cosmetic aspect of scaling is a good side effect, which is the removal of stains on the teeth to make them look whiter and cleaner. Scaling is needed to ensure gum health. Removing those local irritants can do wonders in improving gum health. It is also important in increasing tooth support, minimizing gum bleeding and decreasing bad breath.
Myth: Scaling increasing spaces in between teeth
Fact: Scaling prevents gum disease and bone loss, thus stopping the opening of gaps
It is not impossible to physically move teeth using a scalar. Also, enamel cannot be cut using this machine. This, scaling cannot cause spacing. Spaces seem to appear following a scaling procedure because those spaces have long been there; they were just covered in tartar. Once the disease that causes the tartar is removed, these spaces reappear
So are you now convinced? With all the facts backed by science listed above, now you have no more reason to believe those rumors spread by people who know very little about dental care. Value your oral health and get regular scaling. Remember that your smile is worth more than most of your valuable possessions.
-
When should we start brushing baby teeth?
Start cleaning your child's mouth even before her teeth come in.Wipe the gums off after each feeding with a warm, wet washcloth or a dampened piece of gauze wrapped around your finger. You can also buy thimble-like, soft rubbery devices (they fit over your index finger) to use for rubbing off excess food.
Start cleaning baby's teeth when they appear (6 months) You can start cleaning your baby's teeth by wiping with a soft cloth or brushing with a small soft toothbrush and water. At 18 months start using a pea sized amount of low-fluoride toothpaste to brush your child's teeth.
